The relationship between humidity control and respiratory infection prevention has gained significant attention in recent years, particularly in light of global health concerns. Scientific evidence suggests that maintaining optimal indoor humidity levels can play a crucial role in reducing the transmission of airborne pathogens. This connection stems from how moisture in the air affects both virus survival and human immune defenses. Understanding these mechanisms provides valuable insights for creating healthier living and working environments.
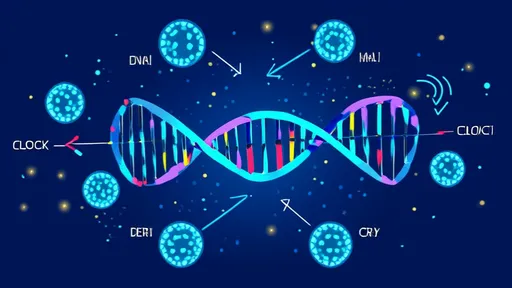
Humidity influences the behavior of respiratory viruses in several ways. Studies have shown that many common viruses, including influenza and coronaviruses, survive longer and spread more easily in dry air. Low humidity causes respiratory droplets to evaporate quickly, transforming them into smaller particles that remain suspended in the air for extended periods. These aerosolized particles can travel farther and penetrate deeper into the respiratory system when inhaled. Conversely, moderate humidity levels between 40-60% appear to create less favorable conditions for viral stability, potentially reducing infection risks.
The human respiratory system's natural defense mechanisms are also humidity-dependent. Mucociliary clearance, the process by which tiny hair-like structures in our airways remove pathogens, functions optimally in properly humidified conditions. Dry air can impair this critical defense system, leaving individuals more vulnerable to infections. Furthermore, research indicates that immune responses at the cellular level may be less effective in extremely dry or humid environments. This dual impact on both pathogens and human physiology makes humidity control a potentially powerful tool in infection prevention strategies.
Building design and ventilation systems play pivotal roles in maintaining healthy humidity levels. Modern construction methods often prioritize energy efficiency, which can sometimes lead to overly dry indoor environments during winter months. Similarly, improperly maintained air conditioning systems in summer may create conditions that are either too dry or encourage mold growth. Architects and engineers are increasingly incorporating humidity control features into building plans, recognizing their importance for occupant health. These include advanced HVAC systems with integrated humidifiers and dehumidifiers that automatically adjust to maintain ideal moisture levels.
Practical solutions for humidity management exist at both institutional and individual levels. Hospitals and healthcare facilities have been early adopters of humidity control measures, particularly in critical care areas. Schools and offices are beginning to follow suit as awareness grows. For home environments, standalone humidifiers and hygrometers offer affordable options for monitoring and adjusting moisture levels. However, experts caution against excessive humidity, which can promote dust mite populations and mold growth - both known triggers for respiratory issues. The key lies in finding and maintaining that beneficial middle range where neither extreme dryness nor excessive moisture prevails.
Emerging technologies are bringing new sophistication to humidity control systems. Smart home devices can now continuously monitor environmental conditions and make automatic adjustments. Some systems even incorporate air purification and humidity control in single units, providing comprehensive protection against airborne threats. Researchers are also developing novel materials that passively regulate humidity through their inherent properties, potentially offering low-energy solutions for maintaining ideal conditions. These advancements promise to make effective humidity control more accessible and efficient across various settings.
The broader implications of humidity control extend beyond individual health benefits. During seasonal outbreaks of respiratory illnesses, proper humidity maintenance in public spaces could theoretically reduce community transmission rates. This possibility has led some public health experts to recommend humidity standards for shared environments similar to existing temperature guidelines. While more research is needed to establish definitive protocols, the potential for humidity management to complement other preventive measures like vaccination and sanitation appears promising. As our understanding of these relationships deepens, humidity control may well become a standard component of holistic infection prevention strategies in homes, workplaces, and healthcare settings worldwide.

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025