In a groundbreaking shift in cancer research, scientists are exploring a radical new approach that could transform how we treat malignant tumors. Rather than aggressively attacking cancer cells with chemotherapy or radiation, researchers are investigating ways to temporarily induce tumors into a dormant state – a biological pause button that could buy precious time for patients and reduce treatment side effects. This emerging field, sometimes called "cancer hibernation therapy," draws inspiration from nature's own survival strategies observed in bears, frogs, and other animals that enter suspended animation during harsh conditions.
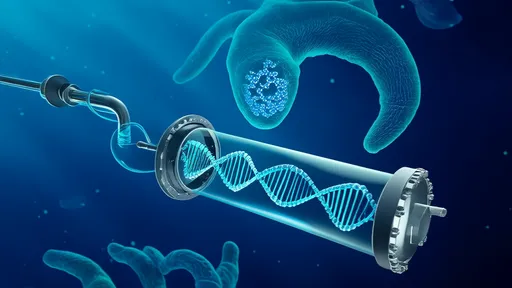
The concept hinges on disrupting the delicate molecular balance that allows cancer cells to proliferate uncontrollably. Recent studies have identified several key pathways that maintain tumor cells in an active, dividing state. By carefully manipulating these pathways – particularly those involving cellular metabolism and stress responses – researchers have successfully triggered reversible dormancy in various cancer types in laboratory settings. Unlike traditional treatments that aim to kill cancer cells (and often healthy cells in the process), this approach seeks to temporarily silence their dangerous behavior.
One particularly promising avenue involves targeting the tumor microenvironment – the complex ecosystem of blood vessels, immune cells, and signaling molecules that surround a cancer mass. Scientists at several leading institutions have demonstrated that altering oxygen levels or nutrient availability can force tumors into a quiescent state remarkably similar to how some animals hibernate during winter months. "We're not eliminating the cancer," explains Dr. Elena Vasquez of the Memorial Cancer Institute, "but we're essentially putting it to sleep in a way that appears to be completely reversible when we want to wake it back up."
The potential clinical applications of this research are staggering. For patients with advanced or metastatic cancers, inducing temporary dormancy could provide critical windows of opportunity – allowing their bodies to recover strength between treatments or giving surgeons time to prepare for complex operations. Early-stage clinical trials are already exploring how short-term tumor hibernation might improve outcomes when combined with existing therapies. In one notable case study, a patient with aggressive pancreatic cancer saw their tumor shrink by nearly 40% after being maintained in a dormant state for six weeks prior to surgery.
Perhaps most remarkably, this approach may help address one of oncology's most persistent challenges: treatment resistance. Many cancers develop ways to evade chemotherapy or targeted drugs, but forcing them into dormancy appears to reset their evolutionary clock. Preliminary data suggests that when tumors reawaken from hibernation, they regain sensitivity to treatments they had previously resisted. This phenomenon, still not fully understood, could revolutionize how we sequence cancer therapies.
As with any emerging medical technology, significant hurdles remain before cancer hibernation becomes standard practice. Researchers must develop precise control mechanisms to ensure tumors remain dormant exactly as long as intended – not waking prematurely nor staying asleep indefinitely. The long-term effects of maintaining cancer cells in this suspended state also require careful study, particularly regarding potential impacts on metastasis. Nevertheless, the field is advancing rapidly, with several pharmaceutical companies now investing heavily in dormancy-inducing compounds.
The philosophical implications of this approach are equally profound. For decades, the war on cancer has been framed as a battle requiring total eradication of malignant cells. Cancer hibernation therapy represents a paradigm shift – the recognition that sometimes, controlling the disease may be more practical than curing it, at least in the short term. As research progresses, we may find that the most effective cancer treatment doesn't involve killing at all, but rather convincing dangerous cells to take an extended time-out until we're better prepared to deal with them.

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025