In the relentless battle against antibiotic-resistant bacteria, scientists are turning to an ancient enemy of pathogens—bacteriophages. These naturally occurring viruses have been silently shaping microbial ecosystems for billions of years. Now, armed with cutting-edge genetic engineering tools, researchers are transforming these microscopic assassins into precision weapons against drug-resistant superbugs.
The rise of antimicrobial resistance (AMR) has been described as a "silent pandemic," with projections suggesting it could claim 10 million lives annually by 2050. Traditional antibiotic development has failed to keep pace with rapidly evolving bacterial defenses. This crisis has spurred renewed interest in phage therapy, a century-old concept that fell out of favor with the antibiotic revolution but may hold the key to combating modern superbugs.
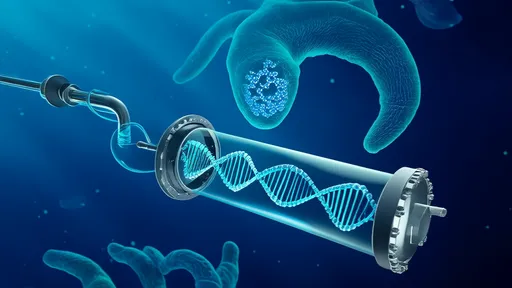
Phage therapy's renaissance comes with a 21st-century twist. Where early practitioners used wild phages as blunt instruments, today's scientists are engineering these viruses with surgical precision. Using CRISPR gene-editing and synthetic biology techniques, researchers can now customize phages to target specific bacterial strains while leaving beneficial microbes unharmed—a crucial advantage over broad-spectrum antibiotics that devastate the human microbiome.
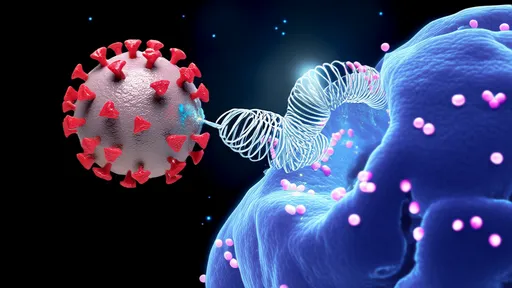
Recent breakthroughs demonstrate phage engineering's potential. At the Massachusetts Institute of Technology, scientists created a "living antibiotic" by modifying T7 phages to carry genes encoding CRISPR-Cas systems programmed to destroy antibiotic resistance genes in E. coli. When tested in mice, these engineered phages selectively killed resistant bacteria while sparing their susceptible counterparts.
The approach offers solutions to two major limitations of natural phage therapy. First, bacteria frequently develop resistance to phages, just as they do to antibiotics. Engineered phages can be designed to attack multiple essential bacterial targets simultaneously, making resistance far harder to evolve. Second, natural phages typically have narrow host ranges, requiring time-consuming matching to specific infections. Synthetic phages can be "broadened" to target entire groups of problematic bacteria.
Clinical applications are already emerging. In 2022, researchers at the University of California, San Diego reported using engineered phages to treat a patient with a persistent Pseudomonas aeruginosa infection that had resisted all antibiotics. The team screened natural phages, then genetically enhanced their ability to penetrate bacterial biofilms—the slimy protective layers that make chronic infections so stubborn. Within weeks, the infection cleared.
Phage engineering also enables innovative delivery strategies. Scientists at the Korea Advanced Institute of Science and Technology have developed "phage bombs"—engineered spores that remain dormant until they encounter specific pathogens in the gut. This could lead to oral phage therapies that survive stomach acid to treat intestinal infections. Other teams are creating phage "cocktails" that combine multiple engineered viruses to prevent resistance and cover more bacterial strains.
The field faces significant challenges. Regulatory pathways for these living medicines remain unclear, as they don't fit traditional drug approval frameworks. Manufacturing engineered phages consistently at scale presents technical hurdles. Perhaps most daunting is the sheer diversity of bacterial pathogens—each may require custom phage solutions, unlike one-size-fits-all antibiotics.
Yet the progress is undeniable. Major pharmaceutical companies, having long abandoned phage research, are now investing in engineered phage startups. The U.S. Biomedical Advanced Research and Development Authority (BARDA) has committed millions to accelerate clinical development. Even the traditional reluctance of Western medicine appears to be softening, with the FDA granting several engineered phage therapies "breakthrough" status.
Environmental applications beyond human medicine may arrive even sooner. Agricultural researchers are testing engineered phages to combat plant pathogens, potentially reducing reliance on chemical pesticides. Wastewater treatment plants could use them to control dangerous bacteria without disrupting the microbial communities essential for processing sewage. Some ventures aim to deploy phage "cleaners" in hospitals to continuously disinfect surfaces from resistant bacteria.
As the technology matures, ethical questions emerge. The same engineering tools could theoretically create harmful phages. Most researchers advocate for strict biosecurity measures and international oversight. There's also debate about how to balance personalized phage therapies with the economic realities of drug development—a tension that echoes the challenges of cancer immunotherapy.
The road ahead will require collaboration across disciplines—from synthetic biology to clinical medicine to regulatory science. But for the first time since antibiotics' golden age, we may be developing tools that can evolve alongside bacterial threats. In nature, phages and bacteria have engaged in an endless arms race for eons. Now, science is tipping the balance in humanity's favor.
As one researcher quipped at a recent microbiology conference, "We're not inventing new weapons—we're just giving the phages better aim." This nuanced approach to an ancient adversary might finally give us the upper hand against superbugs that have outsmarted our best chemical weapons. The age of intelligent phage warfare has begun.

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025